Most of you know that many of my health protocols are based on the health conditions my parents are going through or have gone through.
In fact, the entire reason I started the radio show in August of 2012 was because my mom’s cancer diagnosis in 1995 woke me up in a huge way.
That’s an entire story in and of itself that I’ll share at a later time.
My mom was diagnosed with COPD a few years back and it’s the reason I’m working on the final touches of the COPD Protocol which I hope you find useful.
But the impetus for most of my work is to alleviate the suffering I’m seeing in my parents as they age. 🙁
When I see people suffering with health conditions my heart really goes out to them and I hate seeing people suffer.
I especially hate to see it when I know there are solutions that don’t have side effects but their doctors have them on medications that can sometimes cause permanent damage to tissues.
Let’s get into 4 things you should be aware of if you have COPD.
4 Cautions
Oxalates
Studies suggest that calcium oxalate crystals can deposit in your lung tissue.
Here are some high oxalate foods…. spinach, spinach, beet greens, rhubarb, Swiss chard, almonds, cashews, peanuts, sesame seeds, soybeans, navy beans, black beans, lentils, sweet potatoes, potatoes (with skin), beets, raspberries, blackberries, blueberries, figs, dates, kiwi, oranges, tangerines, starfruit, okra, eggplant, leeks, cocoa powder, dark chocolate, wheat bran, whole wheat flour, quinoa, buckwheat, amaranth, tea (black and green), coffee, turmeric, parsley, celery, and carrots.
The accumulation of these crystals could potentially exacerbating inflammation and oxidative stress, both of which are implicated in COPD pathophysiology. Calcium oxalate may also contribute to tissue damage, scarring, and obstruction of airways in COPD patients. – Source
A Russian study investigating patients with Chronic Obstructive Pulmonary Disease (COPD) and hyperoxaluria examined the impact of oxalates on respiratory obstruction in a cohort of 104 individuals. The researchers observed that insoluble oxalates play a role (the real question is how much of a role though?) in the development of respiratory inflammation and suggested that disruptions in oxalate metabolism may contribute to this inflammatory process. The study concluded that lowering oxalate levels could serve as a potential treatment strategy for managing COPD.
Food Allergies
Food allergies can be connected to COPD through their impact on inflammation and respiratory symptoms. Research indicates that certain allergenic foods can trigger immune responses, leading to inflammation, bronchospasm, and increased mucus production, which exacerbate COPD symptoms.
In a study of 60 COPD patients, significant respiratory symptom improvement was observed when allergenic foods were identified and eliminated from their diets. Pretty amazing right? Some participants also benefited from pollen desensitization, though pulmonary function tests showed only minimal improvements after that was done. The reduction in symptoms was mainly attributed to decreases in bronchospasm, mucosal edema, and mucus production. But still worth exploring.
Atopy and COPD: Overlapping Mechanisms
Studies by Musafiri et al. (2011) discuss the overlap between atopy (a predisposition to allergic conditions) and COPD, emphasizing that food allergies may act as triggers for systemic inflammation, exacerbating COPD symptoms. Allergic responses could lead to airway inflammation, increasing bronchial hyperresponsiveness in COPD patients. – Source
Smoke
Breathing smoke (like my mom who was a life long smoker), whether from cigarettes or environmental sources, is a major risk factor for COPD as it damages lung tissues and causes chronic inflammation. It also causes pulmonary fibrosis and lowers key repair enzymes and alters mineral regulation in your body.
Not good. If you smoke, vape or live in an environment that has poor air quality, I would highly suggest getting a high quality air purifier. Remember, if you don’t have a filter (this goes for water filters too) you are the filter!
Cigarette smoke, in particular (I can still remember running back into the house from the car when my mom asked me to get her her pack of cigarettes! ugh!), leads to the destruction of alveoli (air sacs) and thickening of airway walls, contributing to airflow obstruction and reduced lung function. Environmental smoke, such as from pollution or wildfires, can further irritate your lungs, exacerbate symptoms, and increase your risk of infections, which surprisingly enough accelerates the progression of COPD.
Sugar
Excess sugar intake and insulin resistance are definitely linked to systemic inflammation, which can worsen COPD by increasing lung inflammation and impairing respiratory function. You want to avoid inflammation all over your body. Systemic inflammation puts a burden on every organ, including your lungs. Diabetes is often associated with insulin resistance. It too can exacerbate your COPD symptoms by reducing lung elasticity and heightening the risk of infections.
You want your lungs to be strong yet flexible so that when you breathe your diaphragm expands and contracts allowing more oxygen to be utilized. Poor glycemic control can also impair the repair mechanisms of lung tissues, further contributing to disease progression in COPD patients.
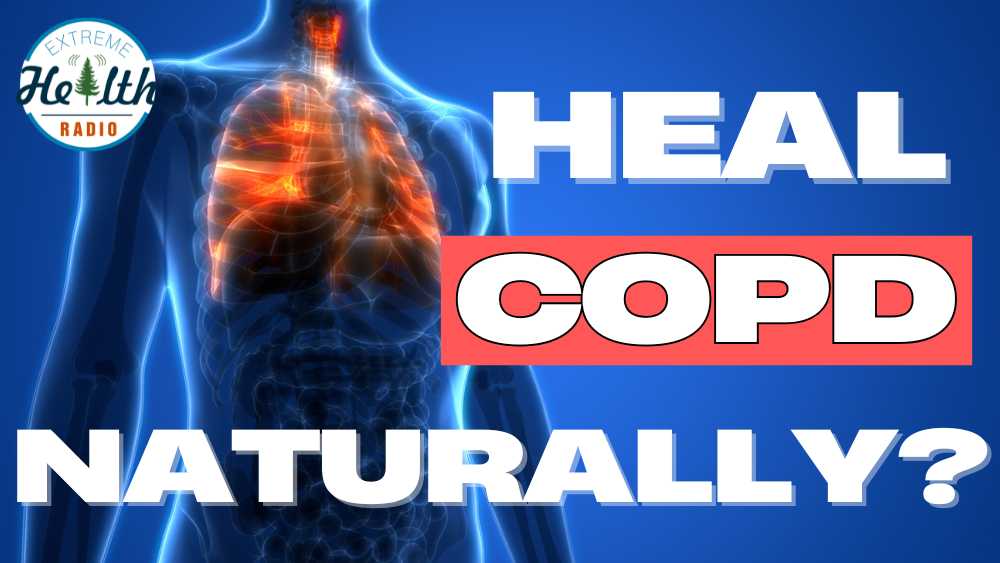
What Is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by persistent airway obstruction, which makes breathing difficult. It encompasses conditions like chronic bronchitis and emphysema, where chronic bronchitis involves inflammation and mucus buildup in the airways, and emphysema damages the air sacs in the lungs, reducing their elasticity and impairing airflow.
Symptoms include coughing, shortness of breath, wheezing, chest tightness, and frequent respiratory infections, often worsening over time. Smoking is the primary cause, but exposure to air pollution, chemical fumes, and genetic factors can also contribute to its development.
In medicine they have to come up with fancy names (many times in latin to make you feel stupid) for a simple condition. Essentially COPD is a progressive (their words not mine) lung dis-ease where the air you breathe is obstructed.
COPD is a broader term which includes other lung conditions like bronchitis, emphysema (which my mom also has from smoking for 35 years) and some people say that COPD is also connected to pulmonary fibrosis, although I haven’t seen much research connecting the two.
9. Natural Ways To Treat COPD
I believe there are not just natural ways to treat COPD but also natural ways to treat just about any health condition. You see modern allopathic medicine using toxic poisons from petrolium is only about 120 years old. Natural healing has been the foundation of how we got here.
It’s not “alternative medicine” it’s the original nature based medicine. The alternative medicine is the allopathic model, which is the new kid on the block pretending to be the only way to heal. I would highly recommend watching the video below for more information on this subject.
1. Stem Cells
Stem cell therapy is where I personally would start as a natural way to treat COPD. There’s a lot of research behind it which I’ll share below. I linked to the Cellular Performance Institute because they’re the world’s leader. I do no know personally if they “treat” specific chronic conditions. I would pursue stem cell therapy from them as a way to improve overall health, not treat a condition.
I invite you to look at some of this research.
Intravenous Allogeneic Mesenchymal Stem Cells for Chronic Obstructive Pulmonary Disease: A Phase 1 Safety Trial
A 2018 study titled “Intravenous Allogeneic Mesenchymal Stem Cells for Chronic Obstructive Pulmonary Disease: A Phase 1 Safety Trial” was conducted at the University of Miami Miller School of Medicine with 62 patients over one year. The results showed that stem cell therapy was safe and reduced inflammation markers, which are key contributors to COPD symptoms. Researchers concluded that MSCs could be a promising approach to improve COPD care while ensuring patient safety – Source.
Stem Cell Therapy for Chronic Lung Diseases: Hope and Reality
In 2019, a study called “Stem Cell Therapy for Chronic Lung Diseases: Hope and Reality” was performed as a collaborative effort in Europe and reviewed multiple small trials involving COPD patients over various durations. The study noted improvements in lung function and reduced disease progression markers, although larger trials were recommended. It concluded that while early results are promising, more robust data is needed to confirm long-term benefits – Source.
Mesenchymal Stem Cells for the Treatment of Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis
The study “Mesenchymal Stem Cells for the Treatment of Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis” published in 2018 analyzed data from human trials involving COPD patients. It highlighted that MSCs could help reduce inflammation and improve overall lung health over treatment periods ranging from months to a year. The researchers emphasized MSCs as a safe and potentially transformative option for COPD management – Source.
2. Ultraviolet Blood Irradiation
I’m a huge fan of UBI or ultraviolet blood irradiation therapy. It has been used in conditions like “septicemia, pneumonia, tuberculosis, arthritis, asthma and even poliomyelitis” (source). I did an entire radio show about it which I’ll post below.
I highly recommend learning about this treatment that got pushed to the side after antibiotics became mainstream. You can’t have people healing themselves naturally can you?
Ultraviolet Blood Irradiation in Chronic Obstructive Bronchitis and Pulmonary Tuberculosis
The first study, titled “Ultraviolet Blood Irradiation in Chronic Obstructive Bronchitis and Pulmonary Tuberculosis”, was conducted in Russia in 1998 with a group of patients suffering from chronic obstructive bronchitis (COB) and pulmonary tuberculosis. Over several weeks, patients experienced improved lung function, increased oxygen levels, and a reduction in inflammatory markers. The researchers concluded that UBI therapy could significantly reduce symptoms and improve respiratory health in COB patients – Source.
Extracorporeal UV Irradiation of Blood in Chronic Nonspecific Lung Diseases
The second study, “Extracorporeal UV Irradiation of Blood in Chronic Nonspecific Lung Diseases”, was conducted in Russia in 1994 with patients suffering from chronic lung diseases, including COPD. The study lasted several weeks and reported better breathing, reduced pulmonary hypertension, and improved oxygen absorption. The conclusion emphasized that UBI therapy provides measurable improvements in respiratory function for patients with chronic lung issues – Source.
3. Cellular Rejuvenation Therapy
Aka “cell therapy” involves injecting a person with animal fetal cells of specific organs with pretty dramatic results. Dr. Paul Niehans injected fetal animal cells from specific organs and tissues into humans and demonstrated remarkable improvements in the corresponding organs and tissues of the recipients. A person is able to learn how to inject themselves with these cells at home if needed.
Personally if I had COPD, this natural therapy would be high on my list. In fact, it’s on my list of natural therapies to do as a maintinence or preventive protocol for my longevity and disease prevention strategy. It’s something you can do if you have a sick or weak organ or if you’d like to extend your life by doing a series of 6 injections once per year.
If this natural way to treat copd sounds interesting to you, I’d read the book linked above or contact the Tahoma Clinic for more information.
Here’s an excerpt from his book Introduction to Cellular Therapy…
“Developments during the last hundred years have led us from Virchow’s cellular pathology to Carrel’s cellular biology and thence to cellular therapy. The foundations of cellular biology were laid by Alexis Carrel, who in numerous experiments demonstrated the undying nature of cells, that is, the perpetual youth of cells, given the right care. He kept alive fragments of the breast of a chicken for 25 years after the death of the bird, without it’s showing any senile changes. Carrell has also studied the influence of healthy cells on diseased cells in the incubator and has observed that dying cells are called back to new life by the addition of the same kind of fresh cells, so great is the regenerative power that wise Nature places in these mysterious cells of fetal and young animals.
From 1931 [the book from which these excerpts were taken was published in 1960] I have systematically practiced cellular therapy on myself and in experiments with animals and I have also practiced it on numerous patients. Today I am in a position to make a survey of some 12,000 which I have carried out in the last 26 years. Cellular therapy is a method of treating the whole organism on a biological basis, capable of revitalizing the human organism with its trillions of cells by bringing to it those embryonic or young cells which it needs. Cells from all organs are at our disposal, the doctor’s art is to choose the right cells. Selective cellular therapy offers new life to the ailing or diseased organism.
Cellular therapy has its roots in the oldest traditions of medicine…in 1400 B.C. the Hindu doctor Susrata recommended Hindus suffering from impotence to eat the sex glands of tigers. Homer relates that Achilles ate the bone marrow of lions in order to increase his strength and his courage…In the third century Chinese doctors prescribed human placenta as a tonic. At the beginning of the sixteenth century, Paracelsus taught that ‘the heart heals the heart; the kidney heals the kidney….’ Hunter in 1771 and Berthold in 1849 demonstrated the substitution effect of testicles grafted on a castrated cock. In 1857 Claude Bernard began to speak of ‘endocrine secretion’. In 1889 Brown-Sequard proved in an experiment on himself the rejuvenating effect of an injection of dog testicle extract. Then surgeons tried grafting animal testicles on man while the endocrinologists, following the example of Brown-Sequard, injected gland extracts subcutaneously.
I myself have carried out more than 1000 transplantations of glands and from 1927 I have been grafting the anterior lobe of the calf on dwarfs, and have had as a result an increase in stature (growth) of as much as 32 centimeters (12.6 inches).”
4. Nebulizing
If you’re not sure what nebulizing is, it’s a way to get liquid medicine inhaled into your lungs. The particle size is micronized so a nebulizer will turn any liquid into a mist that can be inhaled through your nose or mouth, directly into your lungs.
This is a great way in my opinion to bypass your normal digestive organs to get medicine into your blood stream quickly.
The upside is that you bypass normal organs (stomach, liver, gallbladder, intestines) which increases bioavailablity. The other upside is that nebulizing can allow the molecules to directly come in contact with lung tissue.
Nebulizing was first made possible by the medical industry to allow another way for patients to get drugs into their system. The great thing is that we can take one of their devices (a nebulizer) and use it for healing with natural substances that are great for lung health.
If you’re interested I put together the 10 most powerful substances you can nebulize in my Nebulizing For Lung Health protocol.
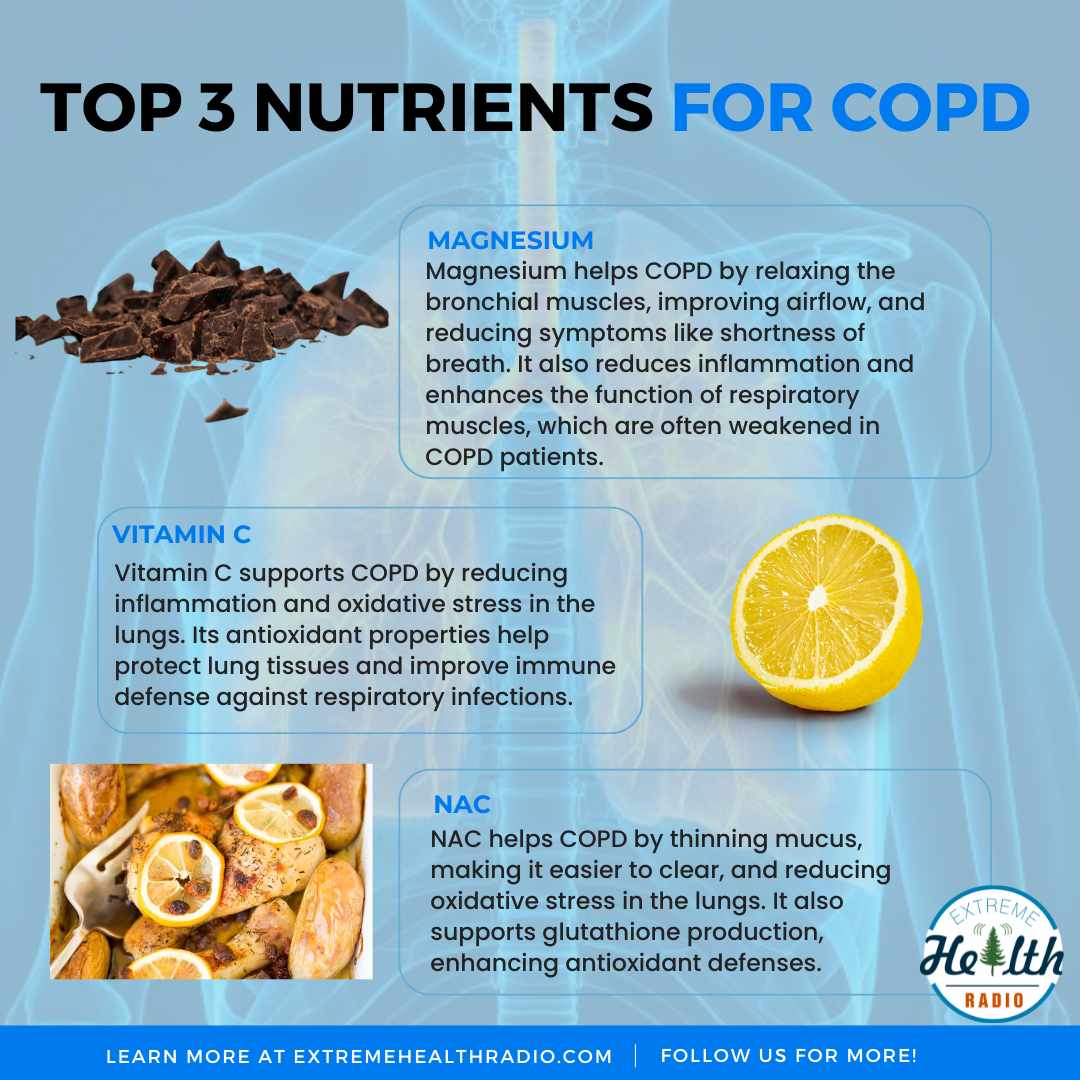
For COPD I like glutathione and N-acetylcysteine (NAC).
The use of nebulized glutathione in the treatment of emphysema: a case report
A 2000 case study published in Alternative Medicine Review evaluated the use of nebulized glutathione in a patient with emphysema over several weeks. The study observed improvements in breathing and symptom relief attributed to glutathione’s role in reducing oxidative stress and replenishing depleted lung antioxidants. Researchers concluded that nebulized glutathione could be a valuable adjunct therapy for managing severe respiratory conditions – Source.
Oral and inhalation usage of acetylcysteine in patients with COPD
A 2019 study in the European Respiratory Journal assessed inhalation use of N-acetylcysteine (NAC) in patients with COPD over a treatment period of months. The study demonstrated that nebulized NAC reduced mucus thickness and airway obstruction, leading to improved respiratory function and decreased disease exacerbations. Researchers highlighted its potential as an anti-inflammatory and mucolytic agent for COPD management – Source.
5. Red Light Therapy
I’m a huge fan of using red light therapy for acute health conditions but also for longevity, disease prevention, energy production, increased metabolism and so much more. I do it daily as part of my long term health maitinence.
It turns out that the wavelengths of the red band of light can penetrate into the lungs and even bones. Red light helps electrons pass more easily across the electron transport chain to cytochrome c-oxidase to make ATP (energy) in the mitochondria.
When your lungs have COPD they are stressed. Stressed cells lead to senesent cells (close to dying) and increasing their energy brings them back to life.
Here’s the red light panel we use right now.
Effect of photobiomodulation in the balance between effector and regulatory T cells in an experimental model of COPD
A 2023 study published in Lasers in Medical Science investigated the effects of red light therapy on COPD patients over eight weeks. The therapy significantly improved lung function, reduced inflammation, and enhanced quality of life, highlighting its potential to alleviate COPD symptoms. Researchers concluded that photobiomodulation offers a promising non-invasive treatment option for managing respiratory conditions – Source.
Effect of photobiomodulation in an experimental in vitro model of asthma-Copd overlap
Another 2023 study in Photobiomodulation, Photomedicine, and Laser Surgery examined low-level laser therapy in COPD patients during a 12-week trial. The results showed reduced oxidative stress and improved exercise tolerance, suggesting that red light therapy can support better lung health and physical activity levels. The study emphasized its safety and efficacy as an adjunct therapy for COPD management – Source.
6. Carbon Dioxide
Much to the dismay of environmentalists it turns out CO2 is incredibly healing to the body. It’s not just a waste gas we breathe out. We did an entire show about CO2 retention which I’ll post below if you’re interested.
An affordable way is to tape your mouth shut when you sleep. Always check with your doctor first about this as I’m not a doctor and this isn’t medical advice. But CO2 is a powerful natural way to treat COPD that most people have never heard before.
If I had COPD I would inhale it using a device called the CarboHaler.
Protective role of carbon dioxide (CO2) in generation of reactive oxygen species
A 2015 study published in Cell Biology International explored the protective role of carbon dioxide (CO2) in reducing reactive oxygen species (ROS) production in cellular systems. It found that increased CO2 levels mitigated oxidative stress, a key factor in COPD progression, by reducing ROS generation. The researchers concluded that CO2 has potential therapeutic benefits in managing oxidative damage in respiratory diseases – Source.
Protective role of carbon dioxide (CO2) in generation of reactive oxygen species
Another 2015 study published in PLOS ONE investigated the effects of therapeutic CO2 inhalation on inflammation and oxidative stress in animal models of lung injury. The study observed reduced markers of inflammation and oxidative damage, suggesting CO2’s potential to protect lung tissue. The authors highlighted its promise as a supportive therapy for conditions involving oxidative stress, including COPD – Source.
7. Lung Exercises
I’m a huge fan of doing lung exercises as they can help retain more oxygen but also increase the elasticity of the lung and aveoli tissue. The other benefit is that lung exercises can actually strengthen lung tissue and surrounding muscles.
Here are a couple of studies you might find interesting.
Successful Extubation of a 29-Week Preterm Neonate with Respiratory Distress Syndrome Following Late Administration of Booster Exogenous Surfactant
The study “Successful Extubation of a 29-Week Preterm Neonate with Respiratory Distress Syndrome Following Late Administration of Booster Exogenous Surfactant” (El Baassiri et al., Authorea Preprints, 2024) is a preclinical observational study. It explored how structured deep breathing exercises improve respiratory efficiency and oxygen saturation in patients with respiratory conditions, including chronic disorders like COPD. The study concluded that incorporating such exercises can significantly enhance pulmonary function. – Source
Novelty of Physiotherapy Management in a Classic Case of Chronic Obstructive Pulmonary Disease in an 84-Year-Old Male Patient with Hypertension and Well-Controlled Hypothyroidism: A Case Report
In the case study “A Comprehensive Case Study of Chronic Obstructive Pulmonary Disease in an 84-Year-Old Male Patient” (Nangliya et al., Cureus, 2024), researchers analyzed the effects of deep breathing and relaxation techniques in an elderly COPD patient. This patient-focused clinical study demonstrated improved lung function, exercise capacity, and quality of life when these techniques were integrated into standard care. It concluded that breathing exercises offer sustained respiratory benefits for COPD management. – Source
8. Salt Inhalation
Did you know that halotherapy can help your lungs function better? What is halotherapy you ask? It’s breathing in micronized particles of salt crystals. The practice has been around for a long time and typically it’s done in controlled environments or in salt mines or salt caves. If I had COPD, I would be doing at least one session per day.
Here are a couple studies you might find interesting…
Salt Halo Therapy and Saline Inhalation Administered to Patients with Chronic Obstructive Pulmonary Disease
The study “Salt Halo Therapy and Saline Inhalation Administered to Patients with Chronic Obstructive Pulmonary Disease: A Pilot Study” (Weinreich et al., J Palliat Care, 2014) is a clinical trial investigating the effects of halotherapy and saline inhalation on COPD patients. This pilot study highlighted improved mucus clearance and reduced respiratory symptoms, concluding that halotherapy may complement standard COPD treatments. – Source
Halotherapy relieves chronic obstructive pulmonary disease by alleviating NLRP3 inflammasome-mediated pyroptosis
The research “Halotherapy Relieves Chronic Obstructive Pulmonary Disease by Alleviating NLRP3 Inflammasome-Mediated Pyroptosis” (Zhang et al., Annals of…, 2022) is a preclinical study exploring halotherapy’s anti-inflammatory and antioxidative effects in COPD. It demonstrated improved lung function and reduced inflammation markers in COPD patients, suggesting halotherapy as a potential adjunctive therapy. – Source
9. Molecular Hydrogen
I’m saving the best biohack for last which is an incredibly powerful natural way to treat COPD. Molecular hydrogen is the smallest known particle in the known universe. Because of its molecule size, weight and density, it’s able to get anywhere into your body. This includes repairing DNA.
Molecular hydrogen is 600x smaller than Vitamin C. It’s incredibly small which makes it very powerful.
As a natural way to to treat COPD I would drink molecular hydrogen water and breathe the gas. In face, I’d sleep with the nasal canula in my nose all night long I believe in it that much. I’ll post a show about molecular hydrogen below. In this show we talked with George Wiseman about molecular hydrogen in general and the AquaCure machine in particular.
There are over 1,000 studies on molecular hyrdrogen on all sorts of health condtions. Here are 2 about natural ways to treat COPD you might enjoy.
The effects of hydrogen treatment in a cigarette smoke solution-induced chronic obstructive pulmonary disease-like changes in an animal model
A 2023 clinical study explored the effects of molecular hydrogen inhalation on patients with chronic respiratory conditions, focusing on its antioxidant and anti-inflammatory properties. The results showed that hydrogen inhalation significantly reduced oxidative stress markers, improved lung function, and alleviated respiratory symptoms, suggesting its potential as an adjunct therapy. – Source
Hydrogen/oxygen therapy for the treatment of an acute exacerbation of chronic obstructive pulmonary disease: results of a multicenter, randomized, double-blind, parallel-group controlled trial
In a 2021 randomized controlled trial, researchers examined the impact of molecular hydrogen on airway inflammation and oxidative damage in individuals with chronic respiratory diseases. The findings indicated that hydrogen therapy effectively reduced inflammation, enhanced pulmonary mechanics, and improved overall patient-reported quality of life, supporting its role in respiratory care. – Source
My Diet & Nutrition Plan For COPD
This plan below is what I would follow as a natural way to treat COPD for me personally. You’ll have to check with your doctor to see what is good for you. Base on my research, these are the supplements I’d add in along with doing all of the other biohacks and health practices I layed out above.
- Diet: General nutritional support with calories, protein, and other essential nutrients. Identify and avoid allergenic foods.
- N-Acetylcysteine: 600–1,200 mg/day in 2–3 divided doses per day.
- Vitamin C: 500–3,000 mg/day.
- Magnesium: 300–600 mg/day.
- Potassium: Increase potassium intake in selected cases, particularly in patients taking diuretics.
Identify and treat iron deficiency. - Nebulized glutathione in selected cases.
Parenteral administration of magnesium and other nutrients in selected cases. - Phosphorus: Monitor serum phosphorus and treat hypophosphatemia.
- L-Carnitine: 1–3 g/day.
- Vitamin A: 5,000–25,000 IU/day.
Conclusion
Obviously this is not a comprehensive approach as I didn’t include Chinese Herbal Medicine aka TCM, herbs, spices, homeopathics or even essential oils. They would all be on the table if I had COPD and wanted to treat it naturally. In fact each one of those that I mentioned could be an entire article in and of itself.
Also not mentioned is making sure you have clean air inside your home and doing what you can to avoid environmental toxins including mold (that’s a deep rabit hole).
I tried to list the most powerful and natural ways to treat COPD that I myself would do.
Let me know if any of these help you. I’d really like to get more people commenting on my articles and sharing what works for you. Thanks for reading!
Questions
- Do you currently have COPD or know somebody that does?
- What symptoms do you have?
- What have you tried? Has it worked?
- What (if anything) has worked?
Comment below!